|
Research Article
Historical trauma, substance use, and mental health symptoms among a sample of urban American Indians
1 Assistant Professor, College of Nursing, University of Nebraska Medical Center, Lincoln, Nebraska, USA
2 Associate Dean of Research, College of Public Health, University of Nebraska Medical Center, Omaha, Nebraska, USA
3 Clinical Assistant Professor, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska, USA
Address correspondence to:
Nicholas Guenzel
Lincoln, Nebraska,
USA
Message to Corresponding Author
Article ID: 100016P13NG2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Guenzel N, Dai HD, Dean L. Historical trauma, substance use, and mental health symptoms among a sample of urban American Indians. Edorium J Psychol 2022;6(2):1–8.ABSTRACT
Aims: Little research has examined historical trauma (HT), addiction, and mental health problems among general populations of urban American Indians (AIs). This study examined associations to help fill this gap.
Methods:This is a secondary analysis of data from a Midwestern urban AI population. Based on a psychological inventory, participants (n=117) were separated into a substance group (n=19), a psychiatric group (n=43), and a control group (n=55). Results of the historical loss scale (HLS, 12 items) and the historical loss-associated symptoms scale (HLASS, 12 items) were examined between the groups.
Results:The psychiatric group reported thinking about three specific losses more than the control group and six specific losses more than the substance group. No significant differences were found between the substance group and the control group. The psychiatric group reported nine historical loss-associated symptoms more frequently than the control group. The substance group reported experiencing five symptoms more frequently than the control group. The substance group reported one symptom more frequently than the psychiatric group.
Conclusion:Historical trauma appears to affect individuals with psychiatric or substance problems differently from those with no problems. American Indians with psychiatric or substance problems report experiencing some HLAS more often than individuals without these problems. The direction of this relationship is unclear, but it is apparent that historical loss thoughts and symptoms likely affect individuals with psychiatric and substance problems differently than the general public. Providers need to be attuned to these results to understand the experiences of their AI patients.
Keywords: American Indian, Mental health, Native American, Substance use
INTRODUCTION
The devastating effects of colonization have been well documented [1]. Colonization has had many deferential impacts on the physical, psychological, and spiritual wellbeing of American Indians (AIs). In addition, colonization has significantly stifled the AI’s socio-economic progress [1]. The pervasive practices of colonization included widespread displacement of AI children from their parents, forcible assimilation, destruction of their environment, and violent massacres that have tried to extinguish their way of life [2]. Some investigators have identified the act of colonization as a form of cultural genocide that has led to HT within the AI population [3],[4]. Several studies have shown that HT can lead to the transmission of intergenerational trauma [5]. This concept explains how serious adverse outcomes can be passed onto future generations over time, which often leads to a pattern of repeated trauma. Unrecognized and untreated HT can heighten the risk for many mental health disorders, addiction issues, sexual abuse, child maltreatment, and domestic violence [5],[6],[7]. It is imperative for providers to fully comprehend the complex phenomenon and nature of HT to address the continuous health disparities among AIs effectively.
The high rate of addiction and mental health problems among many AI groups have been well documented [3]. Furthermore, research has suggested that substance misuse disorders among AIs are strongly associated with HT [4],[8]. Even though a somewhat smaller body of literature has examined HT among AIs, only ten identified studies have examined the convergence of addiction/mental health and HT. Research has found that the combination of HT and addiction/mental health disorders encompasses an array of symptoms [9]. Consequently, this multitude of symptoms often presents significant treatment barriers for AIs [9]. Given the prevalence of both challenges in many AI populations, it is likely that providers can improve the care they give through a better understanding of interactions between these issues [10].
Within many AI communities, problems such as suicide and alcohol misuse are common and persistent issues [10],[11]. American Indians are six times more likely than other races to have suicidal ideations or commit suicide [12]. The AI suicide rate for is 1.32 times higher than the national average among males and 1.5 times higher among females [13]. Suicidality can lead to other impulsive behaviors such as binge drinking or the use of illicit substances [12],[14]. Such behavior may be a method of self-medication to cope with or reduce HT [13],[15]. Studies have shown that AIs have the highest death rates associated with using other illicit substances [14]. AIs have 1.5 times the lifetime rate of an alcohol use disorder compared to whites and 2.1 times the rate of a severe alcohol use disorder in the past 12 months [16]. When compared to any other racial/ethnic group, AIs often have a greater need to receive treatment for their substance misuse disorders [17]. AIs experience psychological distress from mental health issues or cumulative exposure to traumatic events at 1.5 times the general population’s rate [18]. AIs are twice as likely to develop symptoms of post-traumatic stress disorder (PTSD) when compared to other racial ethnicities [18] with a lifetime PTSD prevalence as high as 22.9% compared to 11.7% in the white population [19]. Furthermore, approximately 50% of those with PTSD have additional mental health comorbidities, such as anxiety, depression, bipolar disorder, and other psychoses [19].
Decades of research have established the importance of HT and associated symptoms among AIs in the United States [20]. Most studies on HT among AIs have been conducted on reservations [21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32]. Others have been conducted off reservations but with specific populations such as college students [33],[34]. One identified study was conducted with a general urban population and one with combined reservation and off-reservation adolescents [35],[36]. Many studies provided the breakdown of responses based on the individual HLS and HLASS questions. However, no identified articles have compared individual questions between groups with psychiatric symptoms, addiction, and controls. Knowing the overall rates of HLS and HLASS may help providers develop a general understanding but does not provide insight into the particular loss thoughts and associated symptoms seen at a higher rate in the population they treat.
A limited number of studies have examined the relationship between HT and addiction/mental health. Five identified studies explored mental health and HT. One study found that higher HLSs were associated with elevated anxiety in adolescents [22]. Furthermore, another analysis found that individuals with current anxiety or affective disorder or a lifetime history of PTSD had elevated HLAS but not HLS scores [24]. They found no relationship between conduct or antisocial personality disorders and in either of the HLS or HLAS scores. Two studies found associations between depressive symptoms and elevated HLS scores [30],[34]. In addition, another pertinent analysis found higher HLAS scores among adolescents with depressive symptoms [32].
Six studies have examined the relationships between substance use and HT. One study found that participants with a lifetime diagnosis of substance dependence had significantly higher HLS and HLAS scores [24], while another study found higher HLS scores associated with alcohol use among women [31]. Wiechelt et al. [35] found higher HLS scores associated with alcohol and illicit drug use, excluding the use of cannabis. However, another study found no association between HLS and substance use [28]. In a study of Native Hawaiian college students, the investigators found that HT was negatively associated with substance use [33]. Finally, Soto et al. [36] found a relationship between HT and smoking habits.
This paper aims to examine the convergence of substance/mental health problems and HT/ethnic experience among an urban population of AIs. The study’s specific aims include the following:
- Compare the frequency of historical loss thoughts between urban AIs who met the threshold for clinically significant substance problems, those who met the clinically significant threshold for other mental health problems, and those who did not meet the clinically significant threshold for any mental health problems.
- Compare the frequency of historical loss symptoms between urban AIs who met the threshold for clinically significant substance problems, those who met the clinically significant threshold for other mental health problems, and those who did not meet the clinically significant threshold for any mental health problems.
MATERIALS AND METHODS
Participants were recruited through a booth at local powwows and through contacts of research assistants. AI community members were trained to administer surveys. Responses were entered into a REDCap portal. More complete methods have been described previously [37]. The same data set was used for the current analysis. Participants were placed in the “substance,” “psychiatric,” or “control” groups. Participants who met the threshold for clinically significant substance issues were placed into the substance group. Some of these individuals also met the threshold for clinically significant mental health problems. Participants who met the threshold for at least one clinically significant non-substance mental health problem were placed into the psychiatric group. Participants who did not meet the threshold for any substance or other mental health problems were placed in the control group.
Measures
Demographics included sex, age, and number of years spent on a reservation. The historical loss scale asks respondents how often they think about 12 specific losses such as land, language, and respect for elders. Possible responses include “Never,” “Yearly or at special times,” “Monthly,” “Weekly,” “Daily,” and “Several times a day” [31]. The historical loss associated symptoms scale asks respondents how often they experience 12 specific symptoms (i.e., anger, anxiety, insomnia) when they think about historical losses. Possible responses include “Always,” “Often,” “Sometimes,” “Seldom,” and “Never” [31]. These instruments were administered in a REDCap survey.
We also administered the Achenbach System of Empirically Based Assessment Adult Self Report (ASEBA ASR). The ASEBA ASR is a psychological symptom inventory that assesses competencies, adaptive functioning, behavioral, emotional, and social problems for individuals aged 19–59 years old [38]. The inventory includes 123 close-ended questions, three open-ended questions, and questions on living status and demographics. Responses range from 0 (not true) to 2 (very/often true). This instrument was administered through the ASEBA web-link which calculates t scores with classifications for “normal,” “borderline,” and “clinical” symptom levels.
Analysis
Descriptive statistics included the mean and standard deviation for continuous variables, along with count and percentage for categorical variables, overall and by group. For this analysis, results of the HLS were dichotomized into “weekly or more” and “monthly or less” while results of the HLASS were dichotomized into “Often or more” and “Sometimes or less.” The reliability of HLS and HLAS scales was assessed by Cronbach’s alpha. Demographic variables were compared by group using the general linear model for continuous variables and the Chi-square test for categorical variables. Logistic regression analysis was performed to compare the distribution of HLS and HLAS items by group. Odds ratios and 95% confidence interval were reported.Statistical analyses were performed using SAS 9.4 (Cary, NC), and p-values <0.05 were considered statistically significant.
RESULTS
Demographics
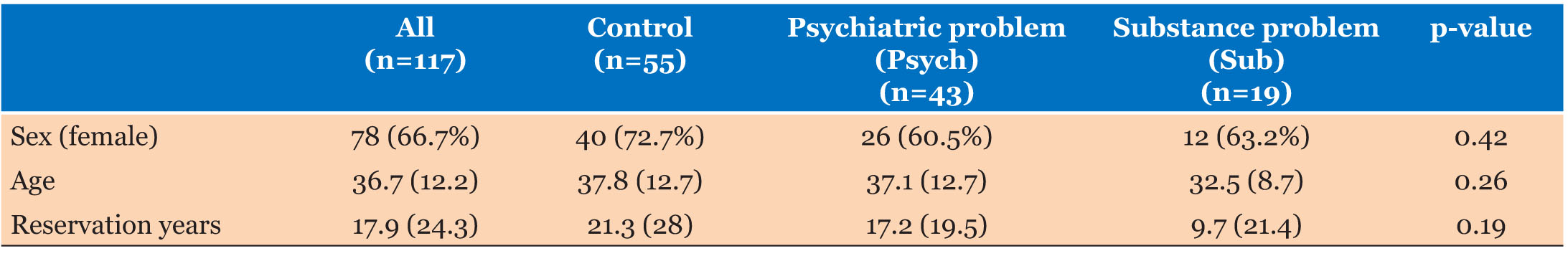
The analytic sample (n=117; age, mean [standard deviation]=36.7[12.2] years; 66.7% female) was classified into three mutually exclusive groups: psychiatric problems (n=43), substance problems (n=9), and no problems (n=55). There were no significant differences between the three groups in proportion of women, mean age, or mean years spent on a reservation (Table 1).
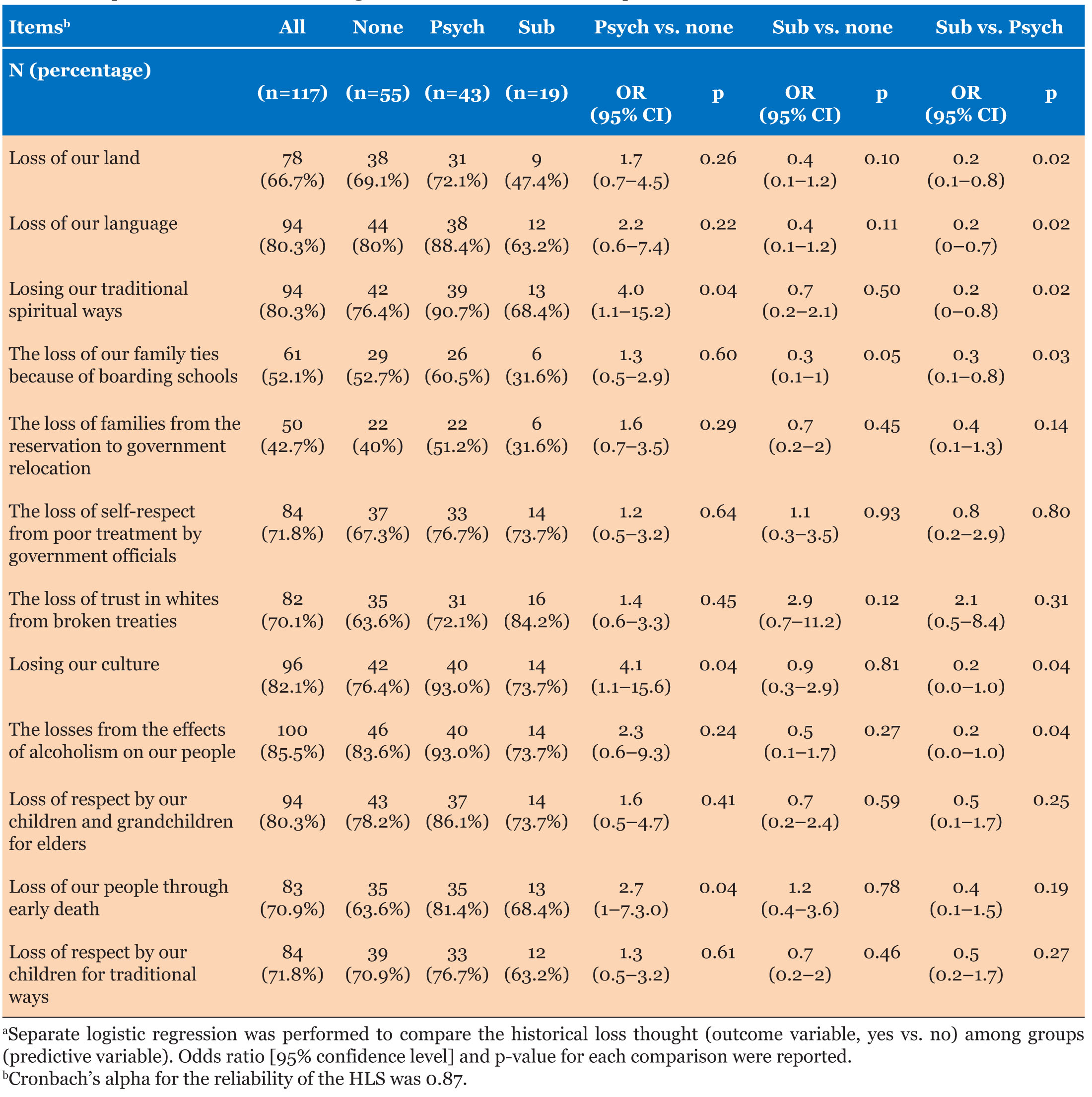
Aim 1. There were relatively few significant differences between the three groups in the prevalence of historical loss thoughts (Table 2). Three significant differences were found in comparisons between the psychiatric and control groups. The psychiatric group reported thinking about losing traditional spiritual ways, culture, and people through early death more frequently than the control group. No significant differences were found between the substance and control groups. The psychiatric and substance groups differed on six of the twelve loss questions. The psychiatric group reported more frequent thoughts on all questions relative to the substance group. The psychiatric group had higher odds of thinking about the losses of land, language, traditional spiritual ways, family due to boarding schools, culture, and losses from the effects of alcoholism than the substance group.
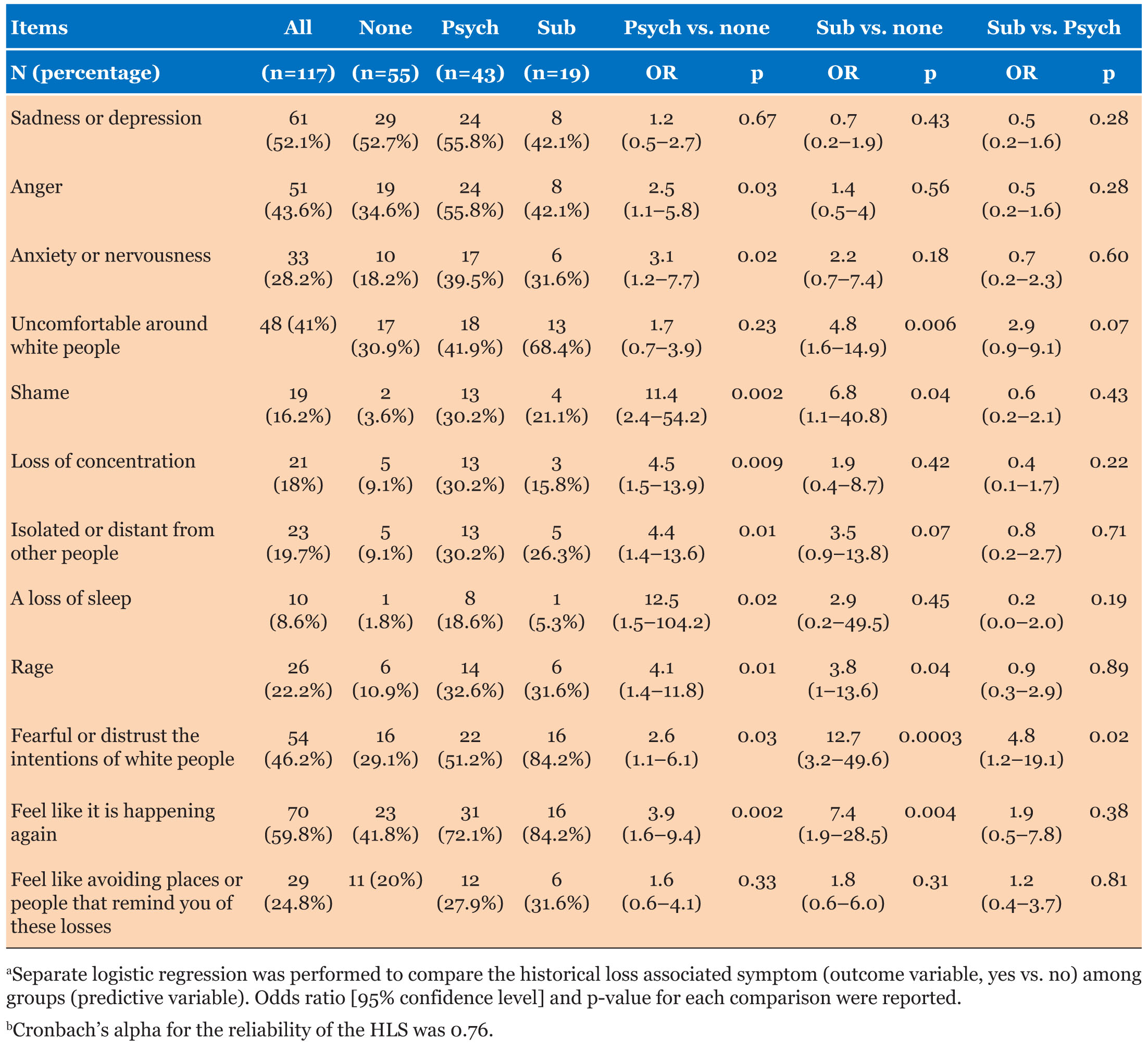
Aim 2. The differences between the three groups regarding HLAS were somewhat more numerous (Table 3). The psychiatric group was more likely to report symptoms on nine of the twelve questions than the control group. These included anger, anxiety or nervousness, shame, loss of concentration, isolation, loss of sleep, rage, fearful or distrusting the intentions of white people, and feeling like the trauma is happening again. In five of the twelve questions, the substance group reported more symptoms than the control group. These included being uncomfortable around white people, shame, rage, fearful or distrusting the intentions of white people, and feeling like the trauma is happening again. The substance group reported higher rates of only one symptom relative to the psychiatric group (fearful or distrusting the intentions of white people).
DISCUSSION
It is difficult to compare the rates of historical loss thoughts and associated symptoms in this sample to previous studies as most publish results do not give responses to the individual questions. However, it can be broadly stated that the rates of historical loss thoughts and associated symptoms were higher in the current study than previous samples. Specifically, having “daily” thoughts was the most common response in this study compared with “yearly” and “never” in other studies [24],[32],[35] except the original study in which “daily” was also the most common response [31]. The historical loss associated symptoms also appear to higher in this study with “sometimes” being the most common response compared to “never” as reported in previous studies [24],[31],[35].
Previous research has found significant associations between substance use, other mental health symptoms, and historical loss thoughts/associated symptoms [4],[8],[9],[22],[24],[30],[31],[32],[33],[34],[35],[36]. However, most previous research has focused on reservation populations leaving providers with relatively minimal insight into the experiences of the majority of AIs, who now live off reservations [21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32]. Additionally, some non-reservation studies have focused on a specific group (i.e., college students) rather than the general population [33],[34],[35],[36]. Lastly, no identified studies provided a frequency analysis of the group’s historical loss thoughts/associated symptoms based on the individual questions. These results inform providers that some of their patients may experience more historical loss thoughts and/or associated symptoms but do not give them insight into which ones may be more frequent among their patients.
Nine of the 36 historical loss thought questions showed significant differences between the groups. More numerous differences may be found with a larger sample size. However, the results reveal some interesting patterns. For all the significant questions, the psychiatric group showed higher rates than the control group. The substance group also had higher rates than the control group. When treating AI patients with psychiatric conditions or substance use disorders, these results may further inform providers about the specific losses that this population often thinks about during their lifetime.
Historical loss associated symptoms may be even more important than the historical loss thoughts from the providers’ perspective. Fifteen of the 36 HLAS showed significant differences between the groups. In nine historical loss thought questions, the psychiatric group showed more frequent thoughts than the control group. The substance group showed more frequent symptoms than the control group in five of the questions. The substance group showed more frequent symptoms in only one question relative to the psychiatric group. All of the significant relationships were in the same direction (i.e., the psychiatric group was more frequent than the control group and the substance group is more frequent than the control group). Perhaps predictably, the three questions that relate most directly to white people all showed significant differences (uncomfortable around white people, fearful or distrusting the intentions of white people, and feeling like the trauma is happening again). This may pose a challenge to providers in this country since most of them are white.
This study has limitations. The sample was relatively small which precludes multivariate analyses and the ability to adjust for other influencing factors. Larger longitudinal studies would help clarify many issues. The sample was also based on a convenience methodology. However, no more systematic methods were available for this urban population. Lastly, the ASEBA ASR focuses on symptoms rather than disorders.
CONCLUSION
Historical loss thoughts and associated symptoms play a significant role in the experience of AIs. This study explored how these affect AIs with psychiatric or substance use problems differently. Providers should learn more about HT and how it may affect their patients. Further research is needed to better comprehend HT among AIs with psychiatric or substance use issues. Specific research in this area can help providers identify ways to improve their quality of care when treating AIs, especially when they embrace an understanding of the complexities involved with HT. Therefore, to facilitate healing, providers need to be mindful and carefully examine the root causes of HT within the AI population. For providers to successfully create culturally specific treatment plans and preventative measures that are therapeutic for this population, they first need to acknowledge the history of AIs and the challenges they have endured.
REFERENCES
1.
2.
3.
Garcia JL. Historical trauma and American Indian/Alaska Native youth mental health development and delinquency. New Dir Child Adolesc Dev 2020;2020(169):41–58. [CrossRef]
[Pubmed]

4.
Smallwood R, Woods C, Power T, Usher K. Understanding the impact of historical trauma due to colonization on the health and well-being of indigenous young peoples: A systematic scoping review. J Transcult Nurs 2021;32(1):59–68. [CrossRef]
[Pubmed]

5.
John-Henderson NA, Ginty AT. Historical trauma and social support as predictors of psychological stress responses in American Indian adults during the COVID-19 pandemic. J Psychosom Res 2020;139:110263. [CrossRef]
[Pubmed]

6.
Cedar Project Partnership, Pearce ME, Christian WM, et al. The cedar project: Historical trauma, sexual abuse and HIV risk among young aboriginal people who use injection and non-injection drugs in two Canadian cities. Soc Sci Med 2008;66(11):2185–94. [CrossRef]
[Pubmed]

7.
Bernards S, Wells S, Morton-Ninomiya M, et al. Buffering effects of social support for indigenous males and females living with historical trauma and loss in 2 first nation communities. Int J Circumpolar Health 2019;78(2):1542931. [CrossRef]
[Pubmed]

8.
Gameon JA, Skewes MC. Historical trauma and substance use among American Indian people with current substance use problems. Psychol Addict Behav 2021;35(3):295–309. [CrossRef]
[Pubmed]

9.
Marsh TN, Coholic D, Cote-Meek S, Najavits LM. Blending aboriginal and western healing methods to treat intergenerational trauma with substance use disorder in aboriginal peoples who live in northeastern Ontario, Canada. Harm Reduct J 2015;12:14. [CrossRef]
[Pubmed]

10.
Morgan R, Freeman L. The healing of our people: Substance abuse and historical trauma. Subst Use Misuse 2009;44(1):84–98. [CrossRef]
[Pubmed]

11.
Whitesell NR, Beals J, Crow CB, Mitchell CM, Novins DK. Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. Am J Drug Alcohol Abuse 2012;38(5):376–82. [CrossRef]
[Pubmed]

12.
Zephier Olson MD, Dombrowski K. A systematic review of Indian boarding schools and attachment in the context of substance use studies of Native Americans. J Racial Ethn Health Disparities 2020;7(1):62–71. [CrossRef]
[Pubmed]

13.
14.
Skewes MC, Blume AW. Understanding the link between racial trauma and substance use among American Indians. Am Psychol 2019;74(1):88–100. [CrossRef]
[Pubmed]

15.
Nutton J, Fast E. Historical trauma, substance use, and indigenous peoples: Seven generations of harm from a “big event”. Subst Use Misuse 2015;50(7):839–47. [CrossRef]
[Pubmed]

16.
Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: Results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry 2015;72(8):757–66. [CrossRef]
[Pubmed]

17.
Myhra LL. “It runs in the family”: Intergenerational transmission of historical trauma among urban American Indians and Alaska Natives in culturally specific sobriety maintenance programs. Am Indian Alsk Native Ment Health Res 2011;18(2):17–40. [CrossRef]
[Pubmed]

18.
McKinley CE, Figley CR, Woodward SM, et al. Community-engaged and culturally relevant research to develop behavioral health interventions with American Indians and Alaska Natives. Am Indian Alsk Native Ment Health Res 2019;26(3):79–103. [CrossRef]
[Pubmed]

19.
Schein J, Houle C, Urganus A, et al. Prevalence of post-traumatic stress disorder in the United States: A systematic literature review. Curr Med Res Opin 2021;37(12):2151–61. [CrossRef]
[Pubmed]

20.
Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, Burrage RL. The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: A systematic review. Am Psychol 2019;74(1):20–35. [CrossRef]
[Pubmed]

21.
Anastario MP, FourStar K, Rink E. Sexual risk behavior and symptoms of historical loss in American Indian men. J Community Health 2013;38(5):894–9. [CrossRef]
[Pubmed]

22.
Armenta BE, Whitbeck LB, Habecker PN. The historical loss scale: Longitudinal measurement equivalence and prospective links to anxiety among north American indigenous adolescents. Cultural Divers Ethnic Minor Psychol 2016;22(1):1–10. [CrossRef]
[Pubmed]

23.
Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, Campbell JC. The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based Native American adolescents and young adults. Am J Community Psychol 2015;55(3–4):411–21. [CrossRef]
[Pubmed]

24.
Ehlers CL, Gizer IR, Gilder DA, Ellingson JM, Yehuda R. Measuring historical trauma in an American Indian community sample: Contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend 2013;133(1):180–7. [CrossRef]
[Pubmed]

25.
Goodkind J, LaNoue M, Lee C, Freeland LR, Freund R. Involving parents in a community-based, culturally-grounded mental health intervention for American Indian youth: Parent perspectives, challenges, and results. J Community Psychol 2012;40(4):468–78. [CrossRef]
[Pubmed]

26.
Whitbeck L, Chen X, Hoyt DR, Adams GW. Discrimination, historical loss and enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American Indians. J Stud Alcohol 2004;65(4):409–18. [CrossRef]
[Pubmed]

27.
Rink E, FourStar K, Elk JM, Dick R, Jewett L, Gesink D. Pregnancy prevention among American Indian men ages 18 to 24: The role of mental health and intention to use birth control. Am Indian Alsk Native Ment Health Res 2012;19(1):57–75. [CrossRef]
[Pubmed]

28.
Spence N, Wells S, George J, Graham K. An examination of marijuana use among a vulnerable population in Canada. J Racial Ethn Health Disparities 2014;1(4):247–56. [CrossRef]
[Pubmed]

29.
Walls ML, Whitbeck L, Armenta B. A cautionary tale: Examining the interplay of culturally specific risk and resilience factors in indigenous communities. Clin Psychol Sci 2016;4(4):732–43. [CrossRef]
[Pubmed]

30.
Walls ML, Whitbeck LB. Distress among indigenous north Americans: Generalized and culturally relevant stressors. Soc Ment Health 2011;1(2):124–36. [CrossRef]
[Pubmed]

31.
Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol 2004;33(3–4):119–30. [CrossRef]
[Pubmed]

32.
Whitbeck LB, Walls ML, Johnson KD, Morrisseau AD, McDougall CM. Depressed affect and historical loss among north American indigenous adolescents. Am Indian Alsk Native Ment Health Res 2009;16(3):16–41. [CrossRef]
[Pubmed]

33.
Pokhrel P, Herzog TA. Historical trauma and substance use among Native Hawaiian College students. Am J Health Behav 2014;38(3):420–9. [CrossRef]
[Pubmed]

34.
Tucker RP, Wingate LR, O’Keefe VM. Historical loss thinking and symptoms of depression are influenced by ethnic experience in American Indian college students. Cultur Divers Ethnic Minor Psychol 2016;22(3):350–8. [CrossRef]
[Pubmed]

35.
Wiechelt SA, Gryczynski J, Johnson JL, Caldwell D. Historical trauma among urban American Indians: Impact on substance abuse and family cohesion. Journal of Loss and Trauma 2012;17(4):319–36. [CrossRef]

36.
Soto C, Baezconde-Garbanati L, Schwartz SJ, Unger JB. Stressful life events, ethnic identity, historical trauma, and participation in cultural activities: Associations with smoking behaviors among American Indian adolescents in California. Addict Behav 2015;50:64–9. [CrossRef]
[Pubmed]

37.
Guenzel N, Struwe L. Historical Trauma, ethnic experience, and mental health in a sample of Urban American Indians[Formula: see text]. J Am Psychiatr Nurses Assoc 2020;26(2):145–56. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Nicholas Guenzel - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hongying Daisy Dai - Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lyndsay Dean - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Nicholas Guenzel et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.